Loading...
Sexual health
Introduction
More than 30 different bacteria, viruses and parasites are known to be transmitted through sexual contact, including vaginal, anal and oral sex. Some STIs can also be transmitted from mother-to-child during pregnancy, childbirth and breastfeeding. Eight pathogens are linked to the greatest incidence of STIs. Of these, 4 are currently curable: syphilis, gonorrhoea, chlamydia and trichomoniasis. The other 4 are incurable viral infections: hepatitis B, herpes simplex virus (HSV), HIV and human papillomavirus (HPV) [1].STIs have a profound impact on sexual and reproductive health worldwide. More than 1 million STIs are acquired every day. In 2020, WHO estimated 374 million new infections with 1 of 4 STIs: chlamydia (129 million), gonorrhoea (82 million), syphilis (7.1 million) and trichomoniasis (156 million). More than 490 million people were estimated to be living with genital herpes in 2016, and an estimated 300 million women have an HPV infection, the primary cause of cervical cancer and anal cancer among men who have sex with men. An estimated 296 million people are living with chronic hepatitis B globally [1].
The UKHSA's latest sexual health annual analysis [2] reports that nationally:
- in 2022, there was a total of 4,394,404 consultations at sexual health services (SHSs), an 8.2% increase compared to 2021 (4,059,608)
- in 2022, there were 2,195,909 sexual health screens (diagnostic tests for chlamydia, gonorrhoea, syphilis or HIV) performed by SHSs, an increase of 13.4% compared to 2021 (1,936,455)
- in 2022 there were 392,453 diagnoses of new STIs among England residents, an increase of 23.8% compared to 2021 (317,022)
- both gonorrhoea and syphilis have returned to the high levels reported in 2019 (prior to the coronavirus (COVID-19) pandemic)
- gonorrhoea is increasing in people of all ages, but the rise is highest among young people aged 15 to 24 years
- infectious syphilis (primary, secondary and early latent) is increasing both among gay, bisexual or other men who have sex with men (GBMSM), and heterosexual people
- chlamydia diagnoses (all ages) increased 24.3% from 160,279 diagnoses in 2021 to 199,233 in 2022
- gonorrhoea diagnoses increased to 82,592 diagnoses in 2022, an increase of 50.3% compared to 2021 (54,961)
- infectious syphilis diagnoses increased to 8,692 diagnoses in 2022, up 15.2% compared to 2021 (7,543)
- first episode genital warts diagnoses decreased in 2022 with 26,079 (8.5% compared to 28,497 in 2021)
- the impact of STIs remains greatest in young people aged 15 to 24 years, GBMSM, and some black ethnic groups
- 690,531 chlamydia tests were carried out in 2022, a 1.2% decrease compared to 2021 (698,979)
- there were 68,882 chlamydia diagnoses, an increase of 21.8% compared to 2021 (56,562) – test positivity increased from 8.1% to 10.0% over the same period
Data Overview
Sexually Transmitted Infections
New STI Diagnoses
Oldham's rate of new STI diagnoses has remained consistently below the regional and national averages for over a decade. Latest 2022 figures reveal Oldham's rate to be 27% lower than the North West rate and 35% lower than the England rate. All three areas saw a decrease in rate during the Covid-19 pandemic and have since experienced an increase, although not yet returning to pre-pandemic rates. Oldham's rate is third lowest across Greater Manchester (out of 10 Local Authorities) and 5th lowest amongst CIPFA neighbours (out of 16 Local Authorities).Figure 1: New STI diagnoses trend
 Source: UK Health Security Agency (UKHSA)
Source: UK Health Security Agency (UKHSA)Figure 2: New STI diagnoses across Greater Manchester
 Source: UKHSA
Source: UKHSA Figure 3: New STI diagnoses amongst CIPFA near neighbours
 Source: UKHSA
Source: UKHSASyphilis
Syphilis is an important public health issue in men who have sex with men (MSM) among whom incidence has increased over the past decade. Oldham's diagnostic rate of Syphilis of 9.9 per 100,000 is lower than the regional rate of 12.7 per 100,000 and the national average of 15.4 per 100,000. Oldham ranks 6th highest across Greater Manchester (out of 10 Local Authorities) and 7th highest amongst CIPFA neighbours (out of 16 Local Authorities). Rates were on the rise up to 2020 and then decreased dramatically during the Covid-19 pandemic. Decreases were also seen regionally and nationally, but the decline in Oldham was more significant. The most recent data from 2022 shows an increase in rate, although Oldham still sits below regional and national comparators.Figure 4: Syphilis diagnostic rate trend
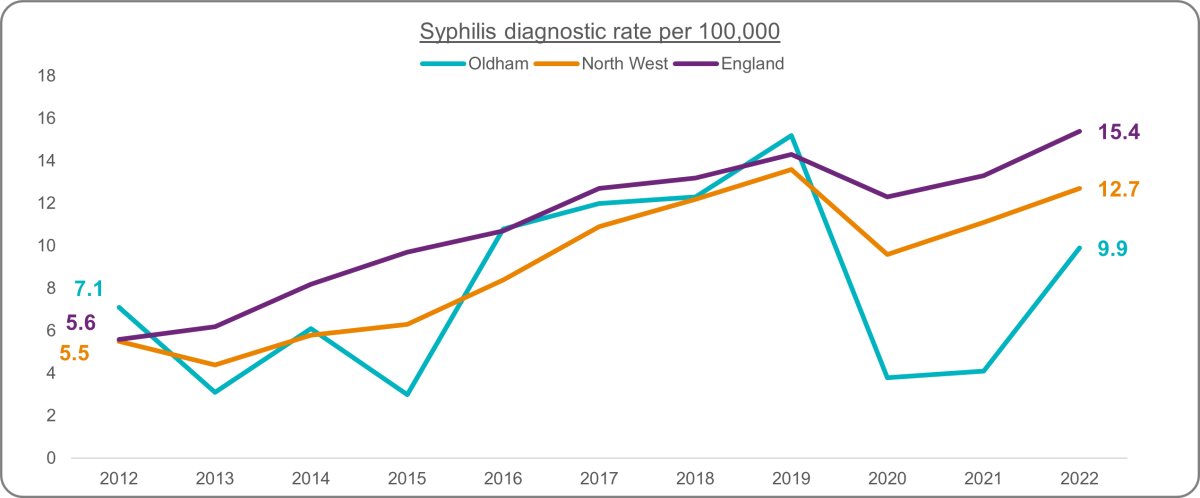 Source: UKHSA
Source: UKHSAFigure 5: Syphilis diagnostic rate across Greater Manchester
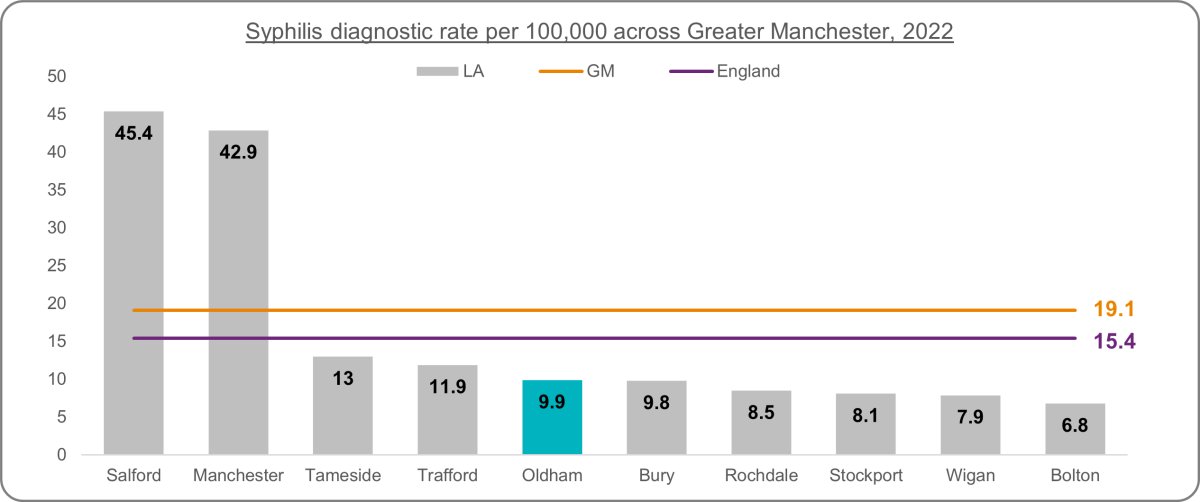 Source: UKHSA
Source: UKHSAFigure 6: Syphilis diagnostic rate amongst CIPFA near neighbours
 Source: UKHSA
Source: UKHSAGonorrhoea
Gonorrhoea causes avoidable sexual and reproductive ill-health. Gonorrhoea is used as a marker for rates of unsafe sexual activity. This is because the majority of cases are diagnosed in sexual health clinics, and consequently the number of cases may be a measure of access to sexually transmitted infection (STI) treatment. Infections with gonorrhoea are also more likely than chlamydia to result in symptoms. Gonorrhoea rates in Oldham are lower than regional and national averages. Rates across Oldham, the North West and England were on a steady increase until the pandemic, when rates declined in 2020 and 2021. Rates regionally and nationally are now slightly higher than in 2019, indicating they are continuing the pre-pandemic upward trend. Oldham's rate has seen an increase in the latest 2022 rate, but the rate has only returned to be equivalent to 2019 rates.Figure 7: Gonorrhoea diagnostic rate trend
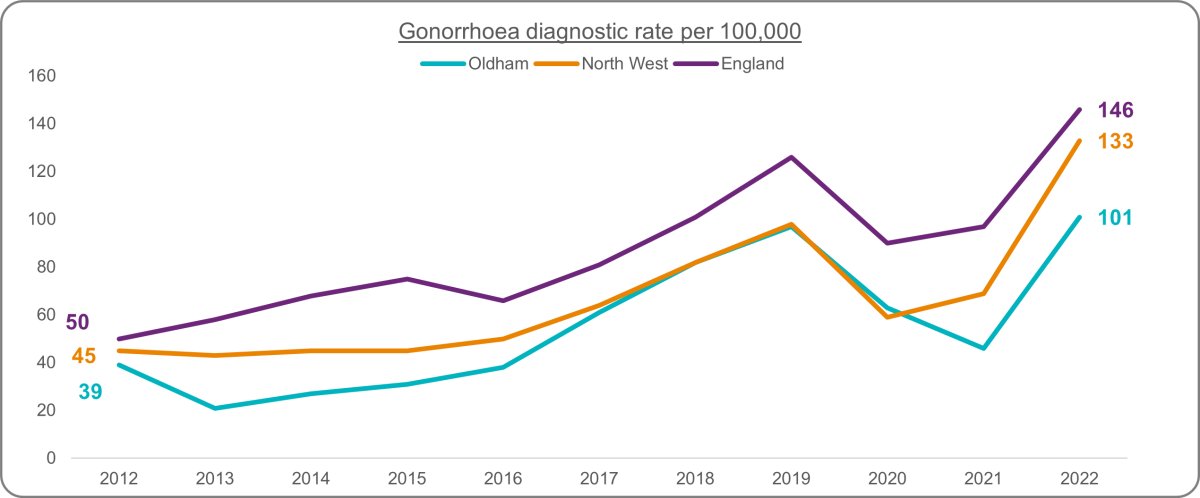 Source: UKHSA
Source: UKHSAFigure 8: Gonorrhoea diagnostic rate across Greater Manchester
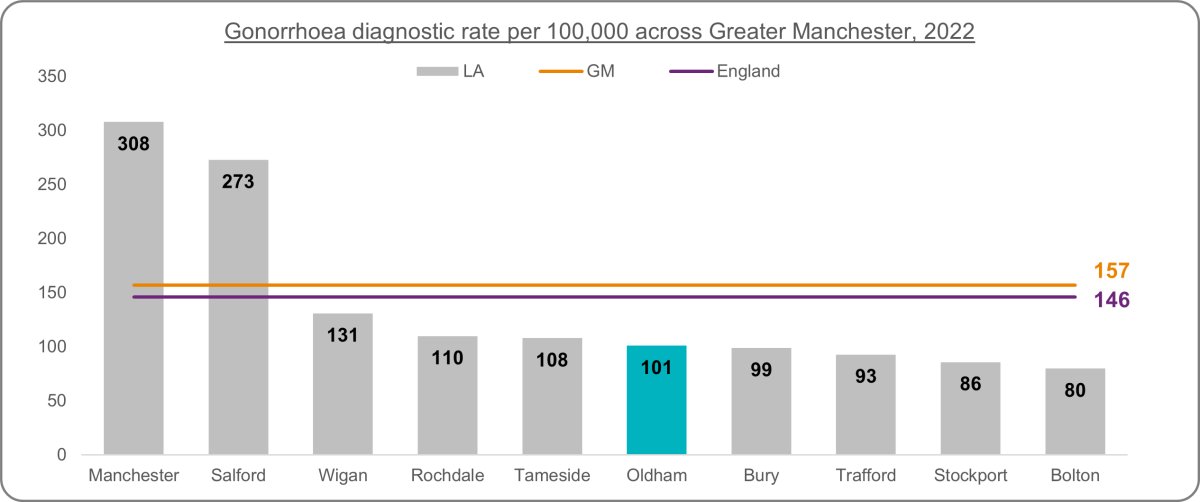 Source: UKHSA
Source: UKHSAFigure 9: Gonorrhoea diagnostic rate amongst CIPFA near neighbours
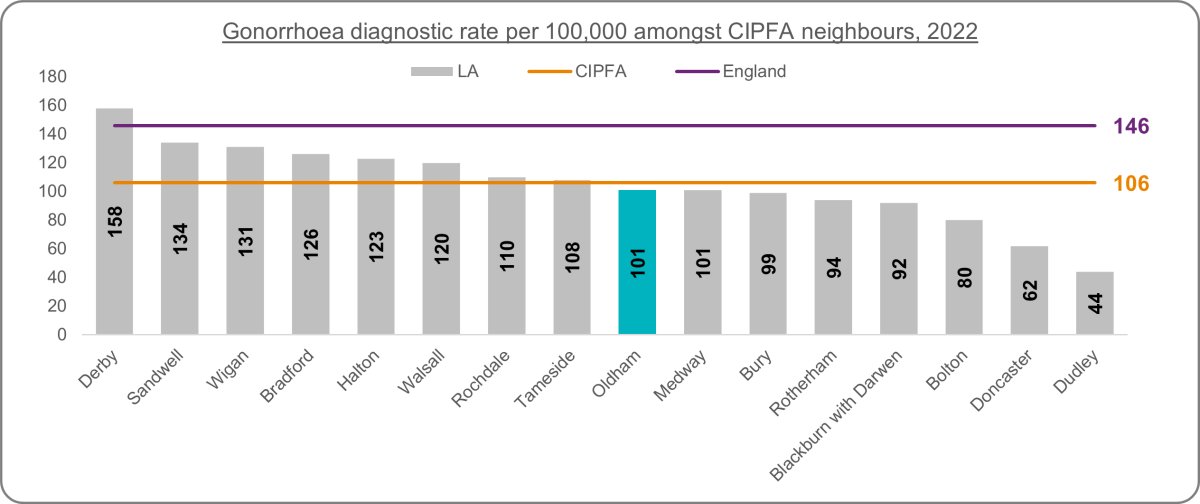 Source: UKHSA
Source: UKHSAChlamydia
Chlamydia is the most common bacterial sexually transmitted infection in England, with rates substantially higher in young adults than any other age group. By diagnosing and treating asymptomatic chlamydia infections, chlamydia screening can reduce the duration of infection, which will reduce an individual’s chance of developing chlamydia associated complications, and also reduce the amount of time someone is at risk of passing the infection on, which in turn will reduce the spread of chlamydia in the population.The National Chlamydia Screening Programme (NCSP) promotes opportunistic screening to sexually active young people aged under 25 years. In June 2021 changes to the programme were announced with a focus on reducing reproductive harm of untreated infection through opportunistic screening offered to young women aged under 25 years. The chlamydia detection rate among under 25 year olds is a measure of chlamydia control activity, aimed at reducing the incidence of reproductive sequelae of chlamydia infection and interrupting transmission. An increased detection rate is indicative of increased control activity; the detection rate is not a measure of morbidity.
Latest 2022 figures show that 12.5% of Oldham's population aged 15 to 24 were screened for Chlamydia, lower than the North West average of 14.2% and the national average of 15.2%. Oldham's rate has fallen below the national rate since 2017. Since 2021, the proportion screened has gradually declined across all areas. The rate in Oldham and the North West has roughly halved, whilst the England rate has decreased by 43%. Oldham ranks 5th highest across Greater Manchester and 9th highest amongst CIPFA neighbours.
Figure 10: Chlamydia proportion aged 15 to 24 screened trend
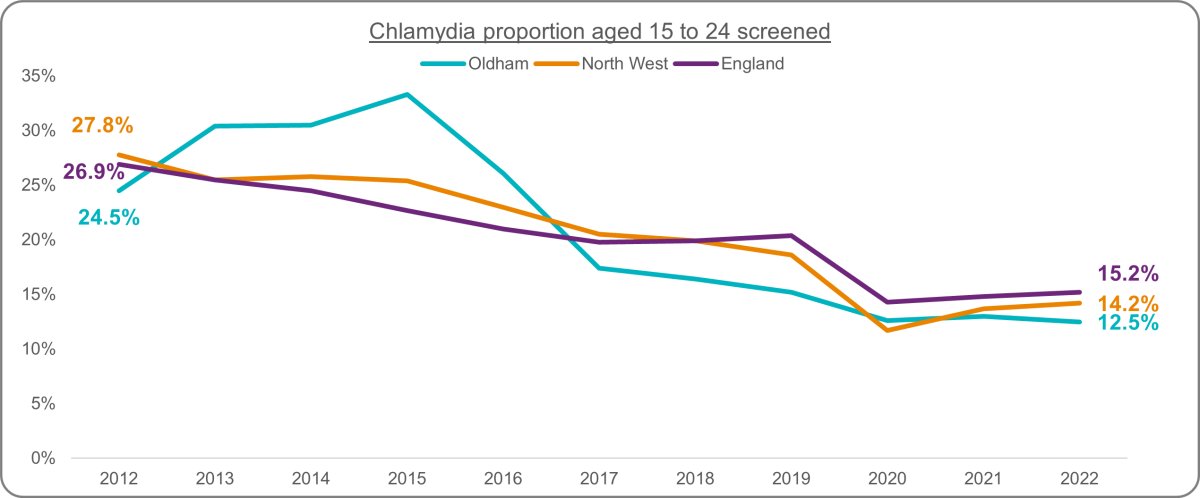 Source: UKHSA
Source: UKHSAFigure 11: Chlamydia proportion aged 15 to 24 screened across Greater Manchester
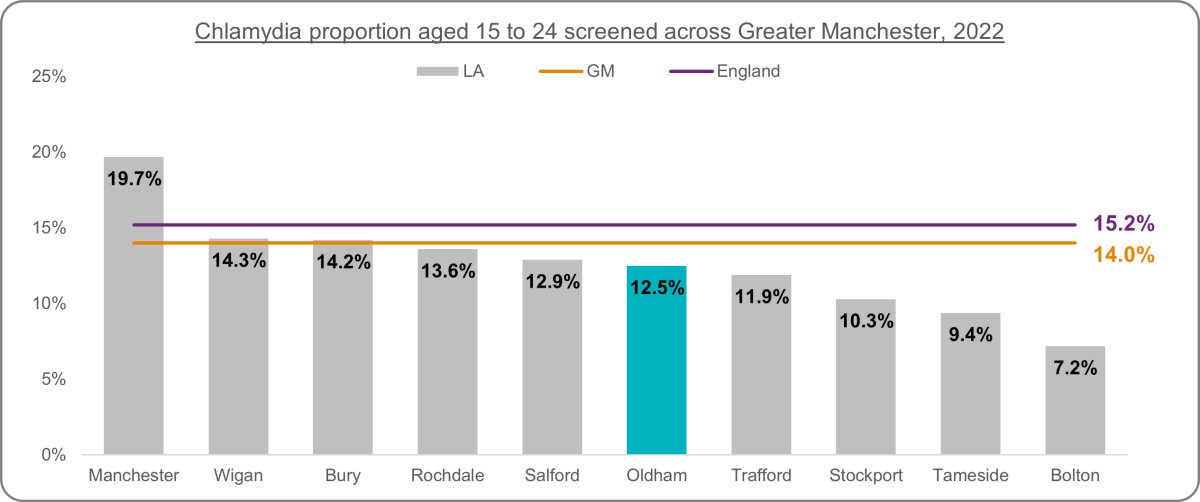 Source: UKHSA
Source: UKHSAFigure 12: Chlamydia proportion aged 15 to 24 screened amongst CIPFA near neighbours
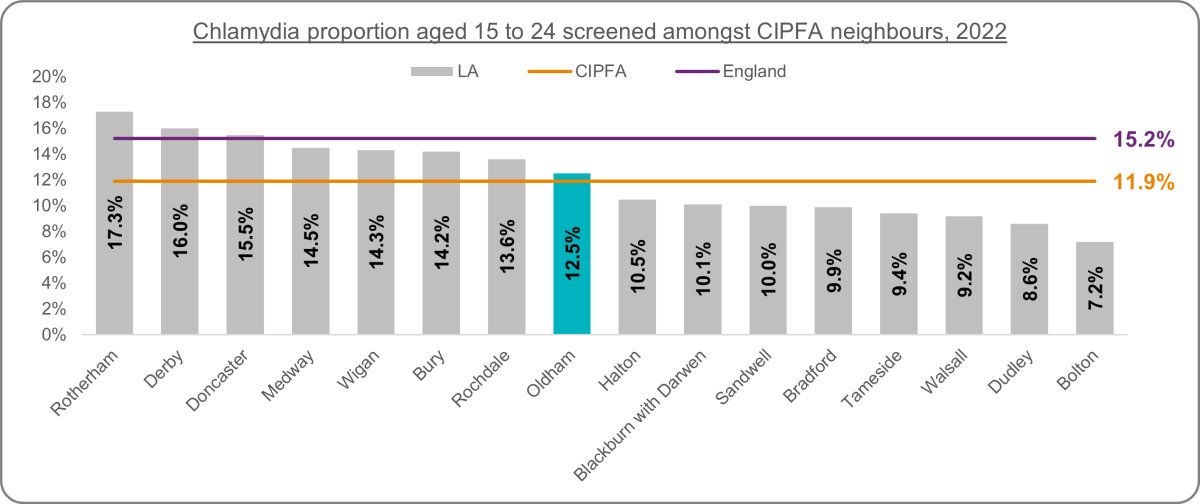 Source: UKHSA
Source: UKHSAThe UK Health Security Agency (UKHSA) recommends that local authorities should be working towards achieving a detection rate of at least 3,250 per 100,000 female population aged 15 to 24. The recommendation was set as a level that would encourage a high volume of screening and diagnoses, be ambitious but achievable and high enough to encourage community screening, rather than specialist sexual health clinic only diagnoses, as well as be likely to result in a continued chlamydia prevalence reduction, according to mathematical modelling.
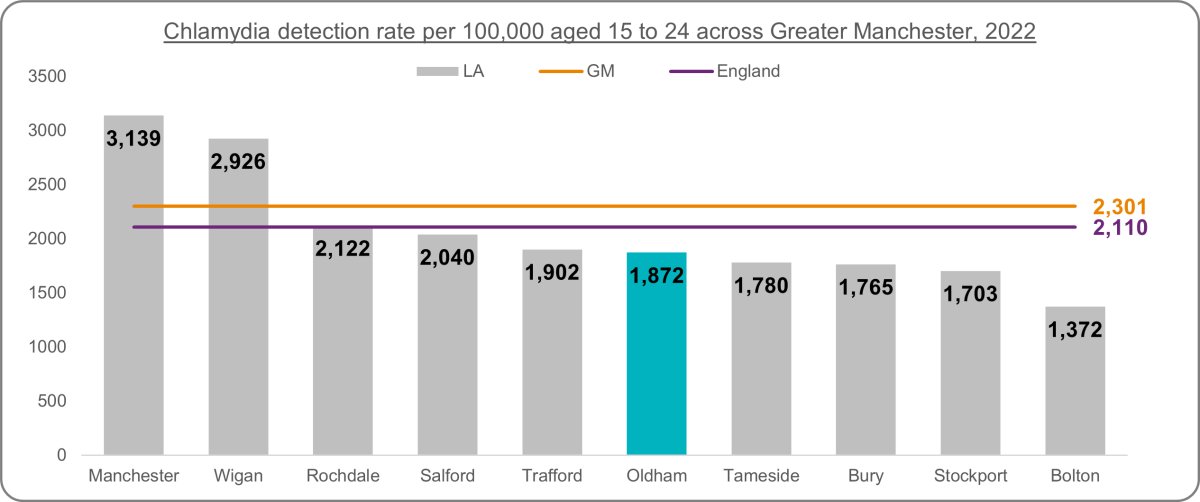
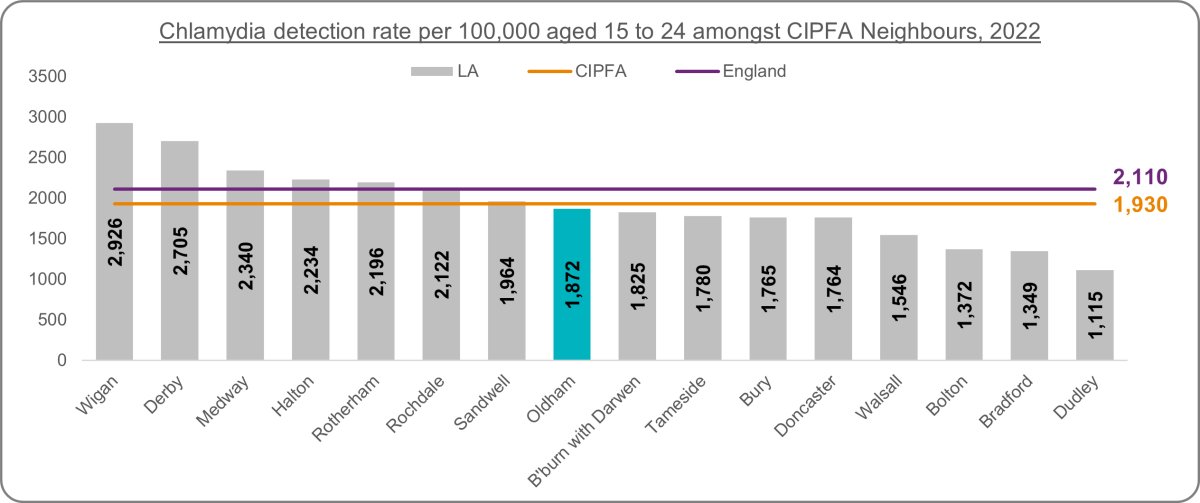
Until 2019, Oldham's rate of Chlamydia detection in females aged between 15 and 24 was higher than regional and national averages. During the pandemic, rates decreased across Oldham, the North West and England. Latest 2022 figures reveal that although increased can be seen against 2021 rates, Oldham's rate is now lower than regional and national rates. Oldham's 2022 rate is 5th highest across Greater Manchester and 9th highest amongst CIPFA neighbours. Oldham, the North West and England along with all Greater Manchester Authorities and CIPFA neighbours fell short of the UKHSA target of a detection rate of at least 3,250 per 100,000. Oldham last met this target in 2017.
Figure 13: Chlamydia detection rate per 100,000 aged 15 to 24 (female) trend
 Source: UKHSA
Source: UKHSAFigure 14: Chlamydia detection rate per 100,000 aged 15 to 24 (female) across Greater Manchester
 Source: UKHSA
Source: UKHSAFigure 15: Chlamydia detection rate per 100,000 aged 15 to 24 (female) amongst CIPFA near neighbours
 Source: UKHSA
Source: UKHSAPopulation Vaccination Coverage: HPV
On the advice of the Joint Committee on Vaccination and Immunisation (JCVI), a HPV national vaccination programme was introduced in 2008, to protect adolescent females against cervical cancer. At that time, a 3 dose schedule was offered routinely to secondary school year 8 females (aged 12 to 13) alongside a catch up programme targeting females aged 13 to 18. In September 2014 the programme changed to a 2 dose schedule based on evidence that showed that antibody response to 2 doses of HPV vaccine in adolescent females was as good as 3 doses. From September 2019, 12 to 13 year old males became eligible for HPV immunisation alongside females, based on JCVI advice.Compared with 2014/15, vaccination coverage has decreased across Oldham, the North West and England, largely impacted by the effects of the Covid-19 pandemic. Compared with 2018/19 data, Oldham's latest data represents a decrease of 33%, whilst England has seen a reduction of 21%. Latest figures show Oldham to be significantly falling behind regional and national rates. Oldham is second lowest across Greater Manchester and third lowest amongst CIPFA neighbours.
Figure 16: HPV vaccination coverage for one dose (12 to 13 years) trend
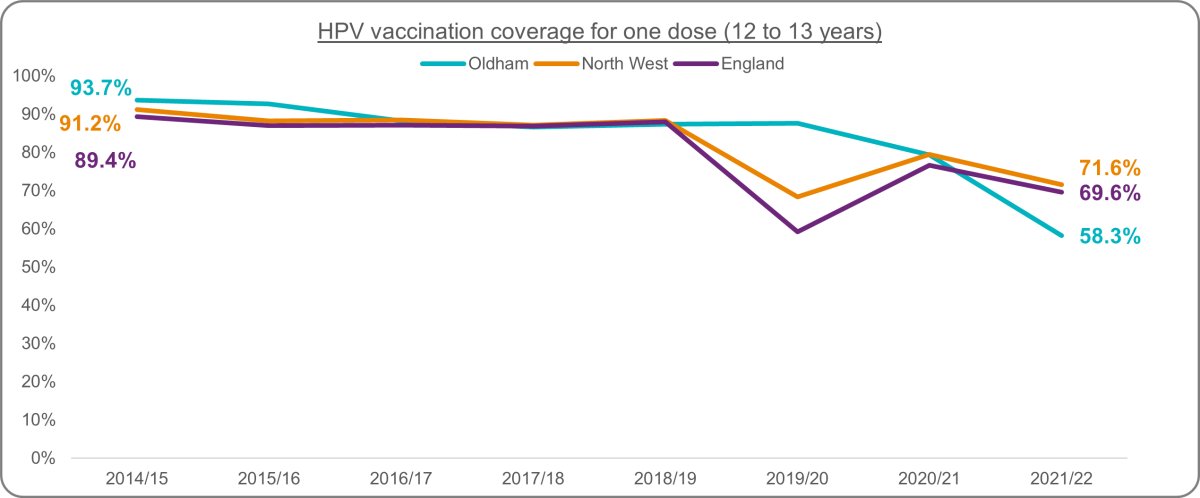 Source: UKHSA
Source: UKHSAFigure 17: HPV vaccination coverage for one dose (12 to 13 years) across Greater Manchester
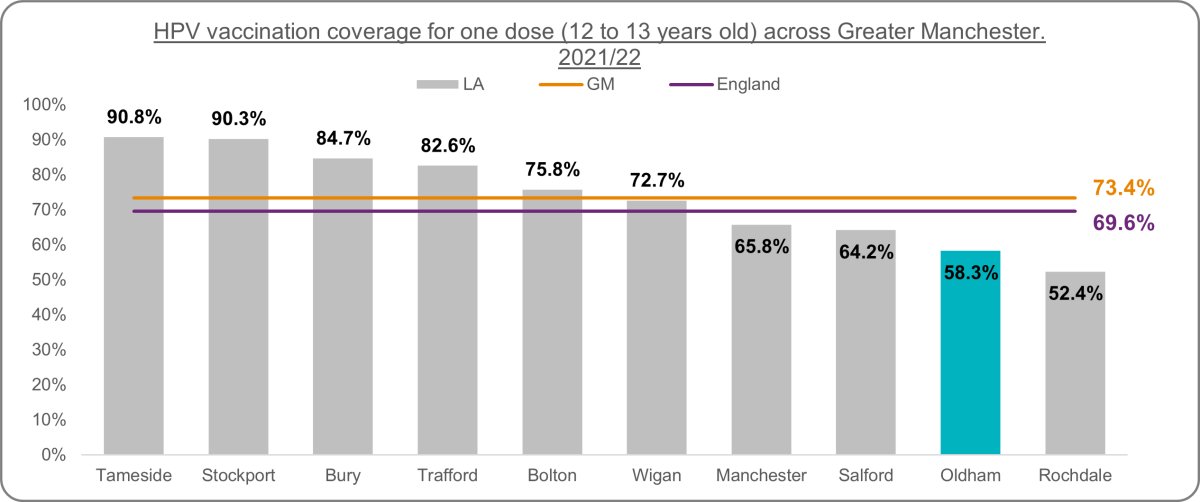 Source: UKHSA
Source: UKHSAFigure 18: HPV vaccination coverage for one dose (12 to 13 years) amongst CIPFA near neighbours
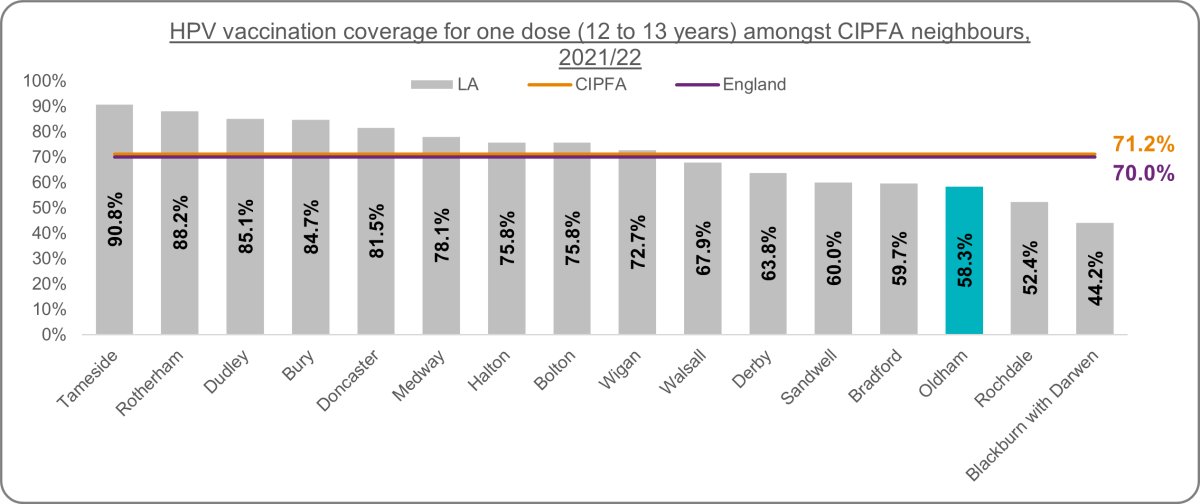 Source: UKHSA
Source: UKHSAHIV
Human immunodeficiency virus (HIV) is an infection that attacks the body’s immune system. Acquired immunodeficiency syndrome (AIDS) is the most advanced stage of the disease. HIV targets the body’s white blood cells, weakening the immune system. This makes it easier to get sick with diseases like tuberculosis, infections and some cancers. HIV is spread from the body fluids of an infected person, including blood, breast milk, semen and vaginal fluids. It is not spread by kisses, hugs or sharing food. It can also spread from a mother to her baby [3].HIV can be treated and prevented with antiretroviral therapy (ART). Untreated HIV can progress to AIDS, often after many years. There is no cure for HIV infection. It is treated with antiretroviral drugs, which stop the virus from replicating in the body. Current antiretroviral therapy (ART) does not cure HIV infection but allows a person’s immune system to get stronger. This helps them to fight other infections. Currently, ART must be taken every day for the rest of a person’s life. ART lowers the amount of the virus in a person’s body. This stops symptoms and allows people to live a full and healthy life. People living with HIV who are taking ART and who have no evidence of virus in the blood will not spread the virus to their sexual partners [3].
NICE HIV testing guidelines define high HIV prevalence local authorities as those with a diagnosed HIV prevalence of between 2 and 5 per 1,000 and extremely high prevalence local authorities as those with a diagnosed HIV prevalence of 5 or more per 1,000 people aged 15 to 59 years. Where diagnosed prevalence exceeds 2 per 1,000, local authorities should implement routine HIV testing for all general medical admissions as well as new registrants in primary care (UK national guidelines for HIV testing 2008).
Oldham's diagnosed HIV prevalence is lower than the North West and England rate and has remained below regional and national comparators for at least the last decade. Oldham is not classified as a 'high prevalence' Local Authority. The North West rate has recently exceeded the 2 per 1,000 threshold and the England rate has been above this threshold consistently for 10 years. Rates have been on a steady increase across all areas, with Oldham seeing a greater increase since 2011 (+59%) compared to the North West (+34%) and England (+19%). Oldham's latest rate is third lowest across Greater Manchester and 8th lowest amongst CIPFA neighbours.
Figure 19: HIV diagnosed prevalence rate per 1,000 trend
 Source: UKHSA
Source: UKHSAFigure 20: HIV diagnosed prevalence rate per 1,000 across Greater Manchester
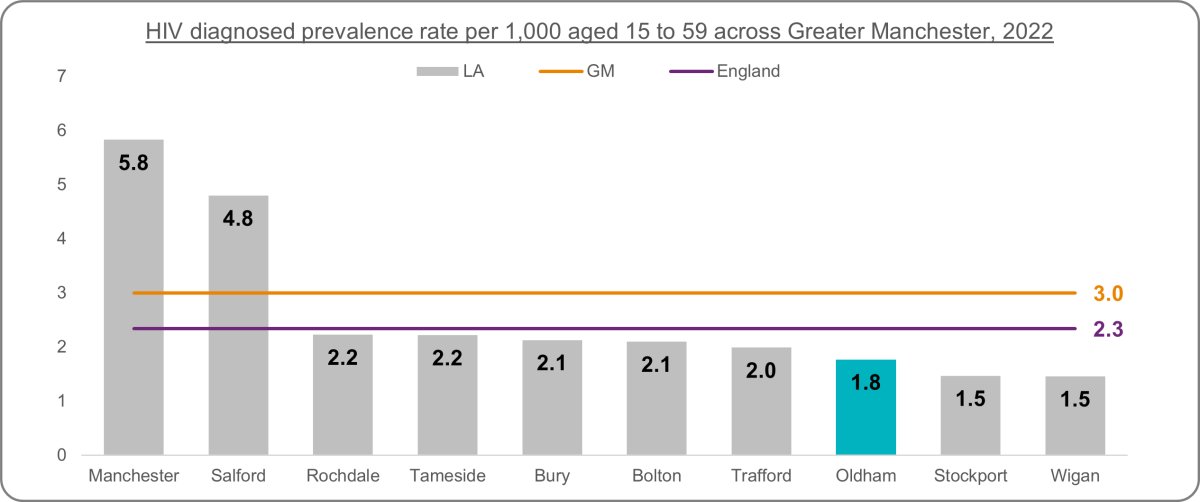 Source: UKHSA
Source: UKHSAFigure 21: HIV diagnosed prevalence rate per 1,000 amongst CIPFA near neighbours
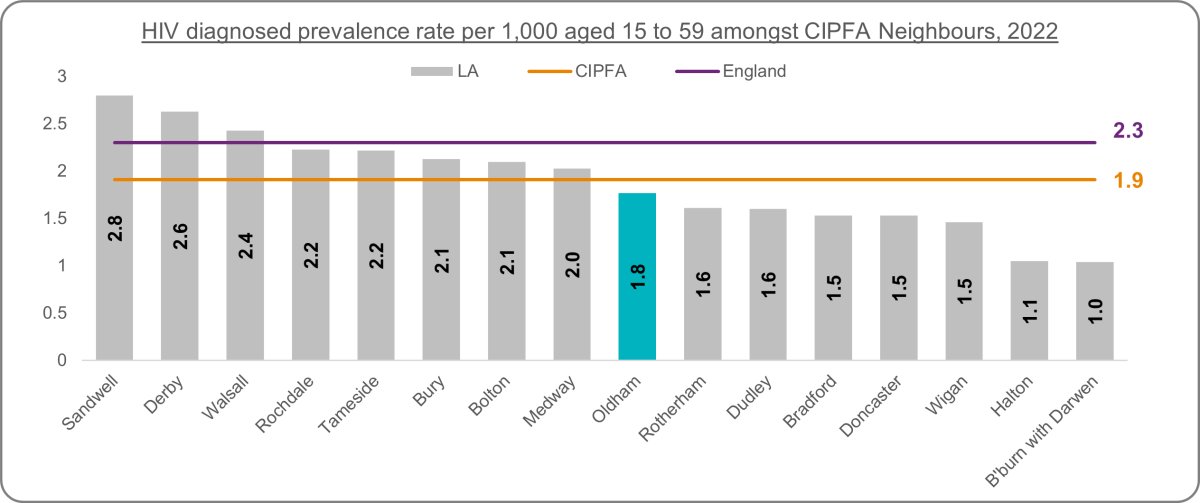 Source: UKHSA
Source: UKHSAHIV testing is integral to the treatment and management of HIV infection. Knowledge of HIV status increases survival rates, improves quality of life and reduces the risk of onward transmission. Until 2020, Oldham's HIV testing coverage was below the North West and England averages, however 2021 and 2022 figures show higher rates. Rates have decreased between 2009 and 2022, with Oldham experiencing a lesser decrease of 15.4% compared with 32% regionally and 30% nationally. Whereas the North West and England experienced a dip in testing during the start of the Covid-19 pandemic, Oldham's rate remained relatively stable between 2019 and 2020. Oldham's latest rate is 4th highest across Greater Manchester and 9th highest amongst CIPFA neighbours.
Figure 22: HIV testing coverage trend
 Source: UKHSA
Source: UKHSAFigure 23: HIV testing coverage across Greater Manchester
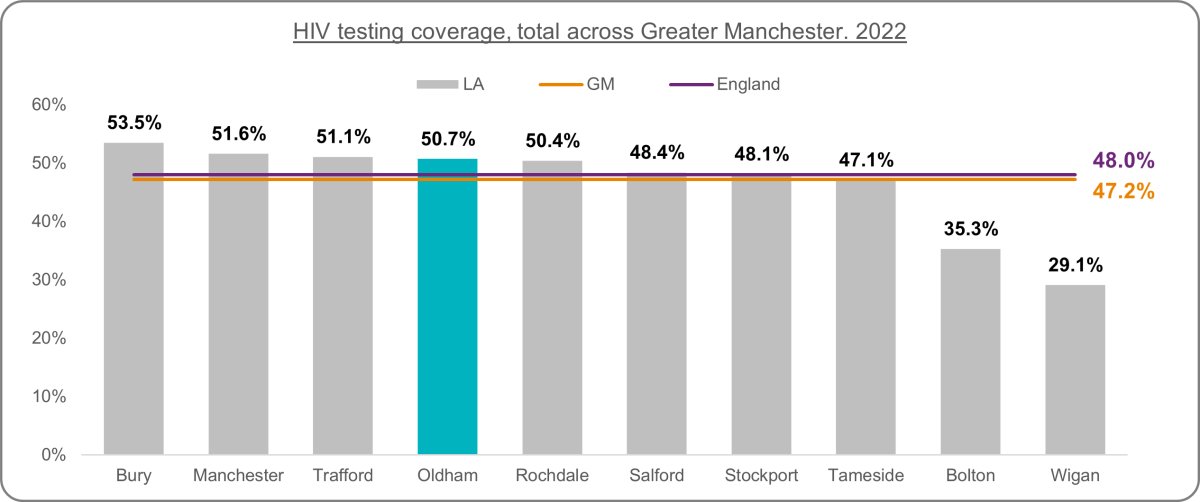 Source: UKHSA
Source: UKHSAFigure 24: HIV testing coverage amongst CIPFA near neighbours
 Source: UKHSA
Source: UKHSAA HIV key strategic priority is to decrease HIV-related mortality and morbidity through reducing the proportion and number of HIV diagnoses made at a late stage of HIV infection. Late diagnosis is the most important predictor of morbidity and mortality among those with HIV infection. Oldham's latest percentage of late HIV diagnoses is higher than regional and national averages. Due to the small numbers involved in these calculations, caution should be exercised when looking at a single data point. Since 2009-11 and with the exception of the 2016-18 data period, Oldham's rate has followed a similar trend to the North West and England. As a result of Oldham's increase in 2020-22, the latest figures show Oldham to be highest across Greater Manchester and third highest amongst CIPFA neighbours. Close monitoring of this indicator is required going forward.
Figure 25: HIV late diagnosis in people first diagnosed in the UK trend
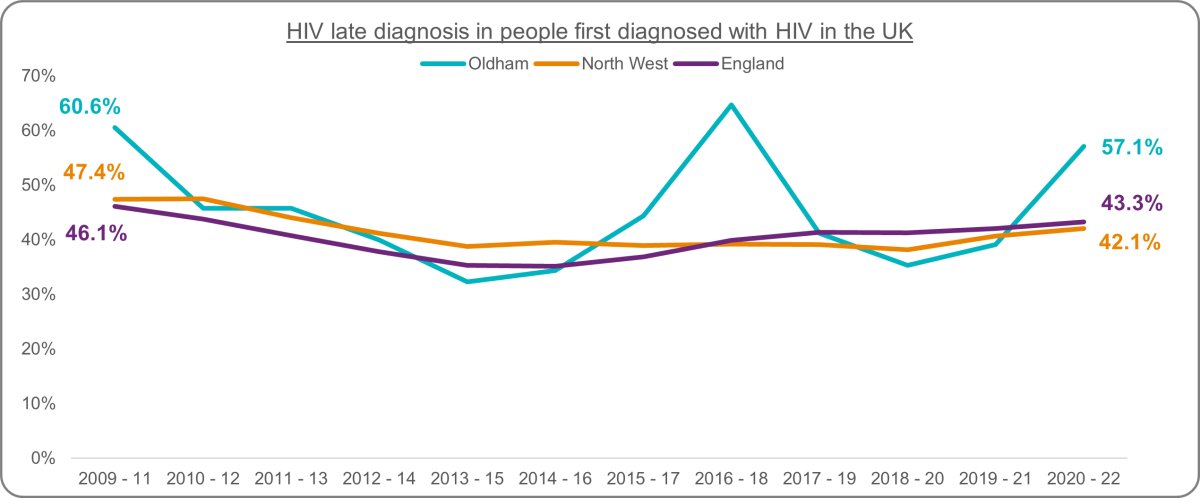 Source: UKHSA
Source: UKHSAFigure 26: HIV late diagnosis in people first diagnosed in the UK across Greater Manchester
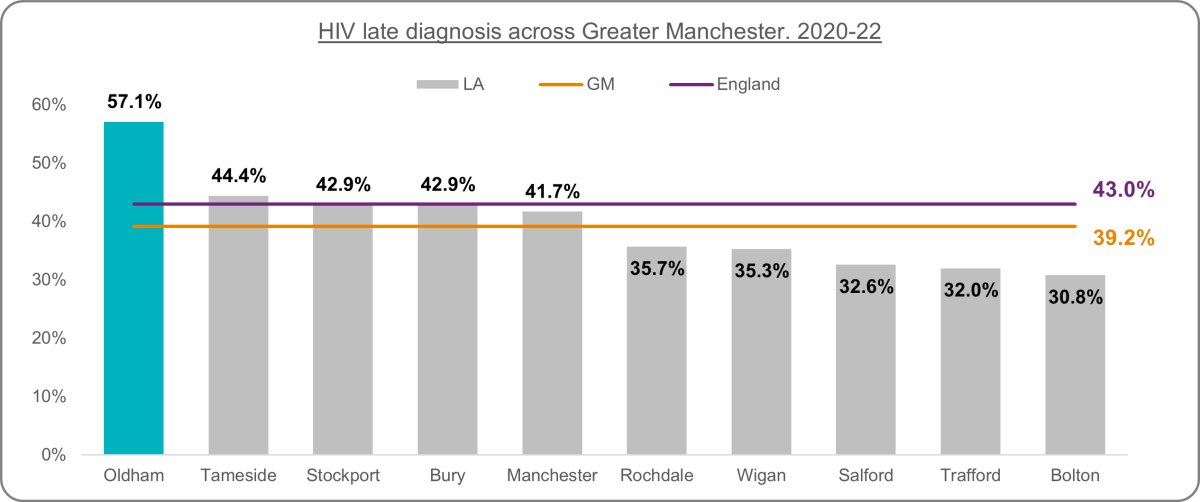 Source: UKHSA
Source: UKHSAFigure 27: HIV late diagnosis in people first diagnosed in the UK amongst CIPFA near neighbours
 Source: UKHSA
Source: UKHSAReproductive Health
The rate of abortions within a population is an indicator of lack of access to good quality contraception services and advice, as well as problems with individual use of contraceptive method. Oldham's total abortion rate is higher than regional and national averages. Since 2012, there have been increases in rates seen across all areas. Oldham's increase of 40% is higher than the increase across the North West (31%) and England (16%). Oldham ranks 5th highest across Greater Manchester and 6th highest amongst CIPFA near neighbours.Figure 27: Total abortion rate per 1,000 trend
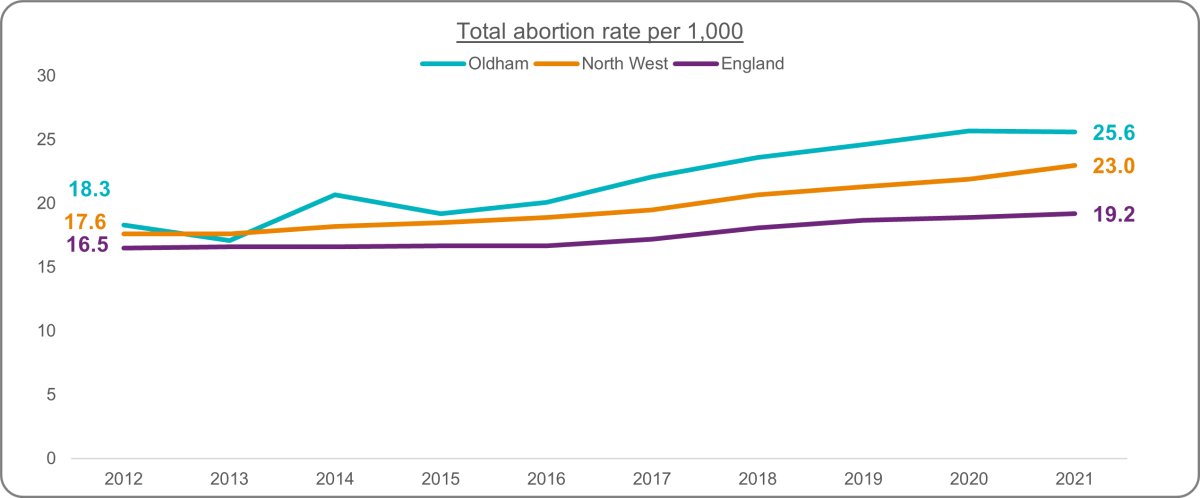 Source: UKHSA
Source: UKHSAFigure 28: Total abortion rate per 1,000 across Greater Manchester
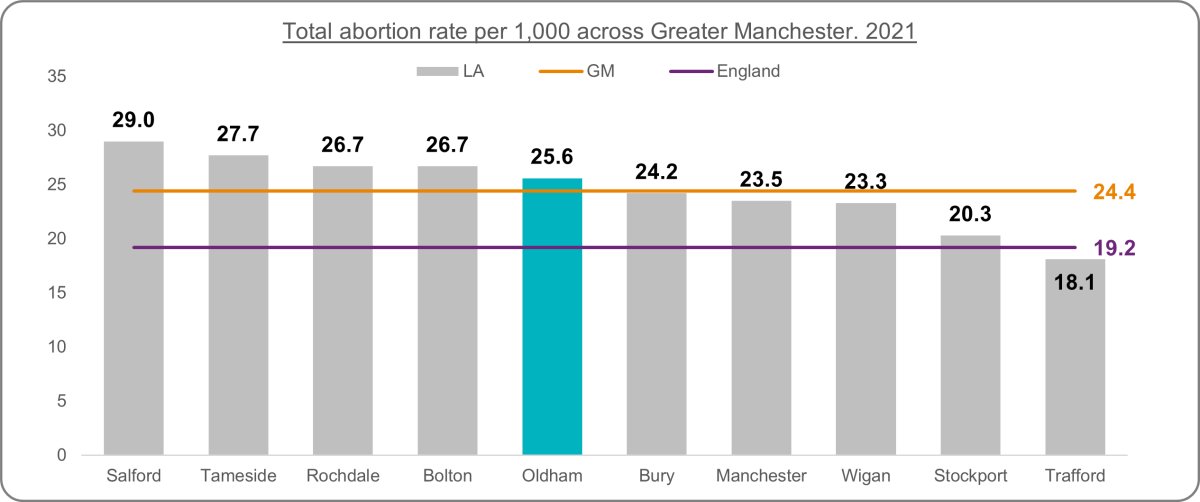 Source: UKHSA
Source: UKHSAFigure 29: Total abortion rate per 1,000 amongst CIPFA near neighbours
 Source: UKHSA
Source: UKHSAThe earlier abortions are performed the lower the risk of complications. Prompt access to abortion, enabling provision earlier in pregnancy, is also cost-effective and an indicator of service quality. Oldham's percentage of abortions performed at under 10 weeks gestation is higher than the North West and England averages. Rates are consistently increasing across all areas. Oldham ranks 3rd highest across Greater Manchester and 3rd highest amongst CIPFA neighbours.
Figure 30: Abortions under 10 weeks (%) trend
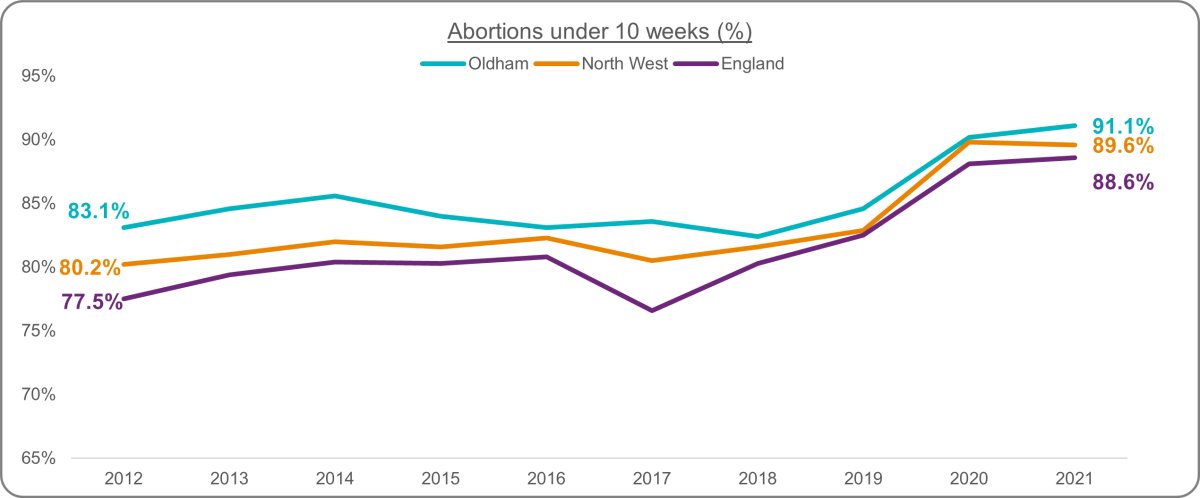 Source: Office for Health Improvement and Disparities, Department of Health and Social Care based on data from abortion clinics
Source: Office for Health Improvement and Disparities, Department of Health and Social Care based on data from abortion clinicsFigure 31: Abortions under 10 weeks (%) across Greater Manchester
 Source: Office for Health Improvement and Disparities, Department of Health and Social Care based on data from abortion clinics
Source: Office for Health Improvement and Disparities, Department of Health and Social Care based on data from abortion clinicsFigure 32: Abortions under 10 weeks (%) amongst CIPFA near neighbours
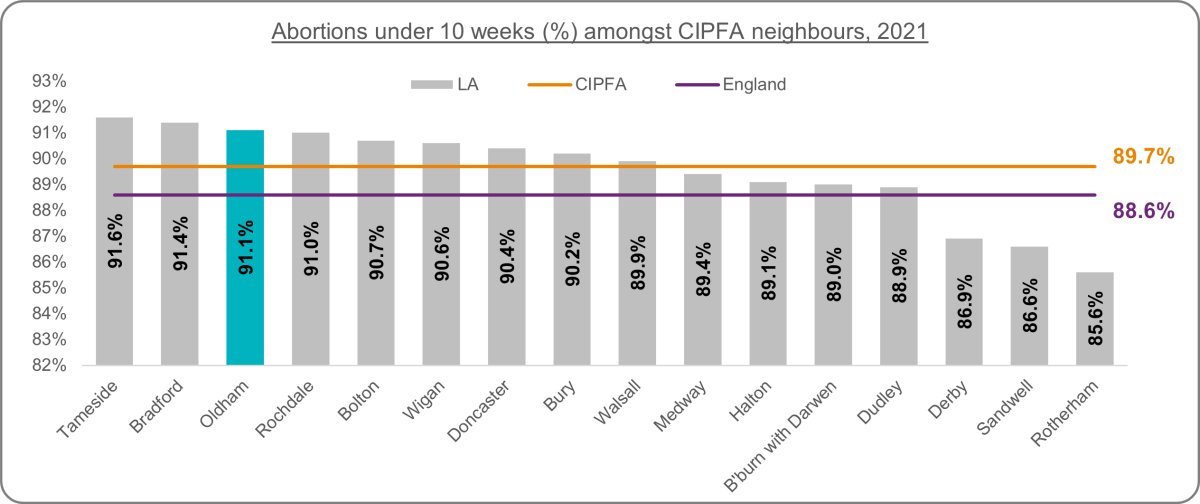 Source: Office for Health Improvement and Disparities, Department of Health and Social Care based on data from abortion clinics
Source: Office for Health Improvement and Disparities, Department of Health and Social Care based on data from abortion clinicsFurther Information & Resources
World Health Organisation Fact Sheets:UKHSA Annual Sexual Health Report
This report provides a descriptive analysis of data on sexually transmitted infections (STIs) diagnoses and screening for chlamydia in England from January to December 2022. It focuses primarily on the changes between 2021 and 2022 and also contains some trend data from 2018 to 2022.
UKHSA Sexually transmitted infections (STIs): annual data tables
Information on STI diagnoses and sexual health services provided in England by demographic characteristics and geographical region.
NICE HIV Testing Guidance
This guideline covers how to increase the uptake of HIV testing in primary and secondary care, specialist sexual health services and the community. It describes how to plan and deliver services that are tailored to the local prevalence of HIV, promote awareness of HIV testing and increase opportunities to offer testing to people who may have undiagnosed HIV.
Teenage Conceptions JSNA Web Page
For data and information relating to teenage conceptions in Oldham
References
[1] World Health Organisation STI Fact Sheet, accessed December 2023, https://www.who.int/news-room/fact-sheets/detail/sexually-transmitted-infections-(stis)[2] UKHSA sexually transmitted infections and screening for chlamydia in England 2022, accessed December 2023,https://www.gov.uk/government/statistics/sexually-transmitted-infections-stis-annual-data-tables/sexually-transmitted-infections-and-screening-for-chlamydia-in-england-2022-report
[3] World Health Organisation HIV & Aids Fact Sheet, accessed December 2023, https://www.who.int/news-room/fact-sheets/detail/hiv-aids

